Spondylolisthesis
Introduction:
Forward translation of one vertebra on another in the sagittal plane of the spine. Whereas spondylolysis was defect in pars interarticularis of lumbar vertebra, commonly due to repeated and increased stress on the pars interarticularis.
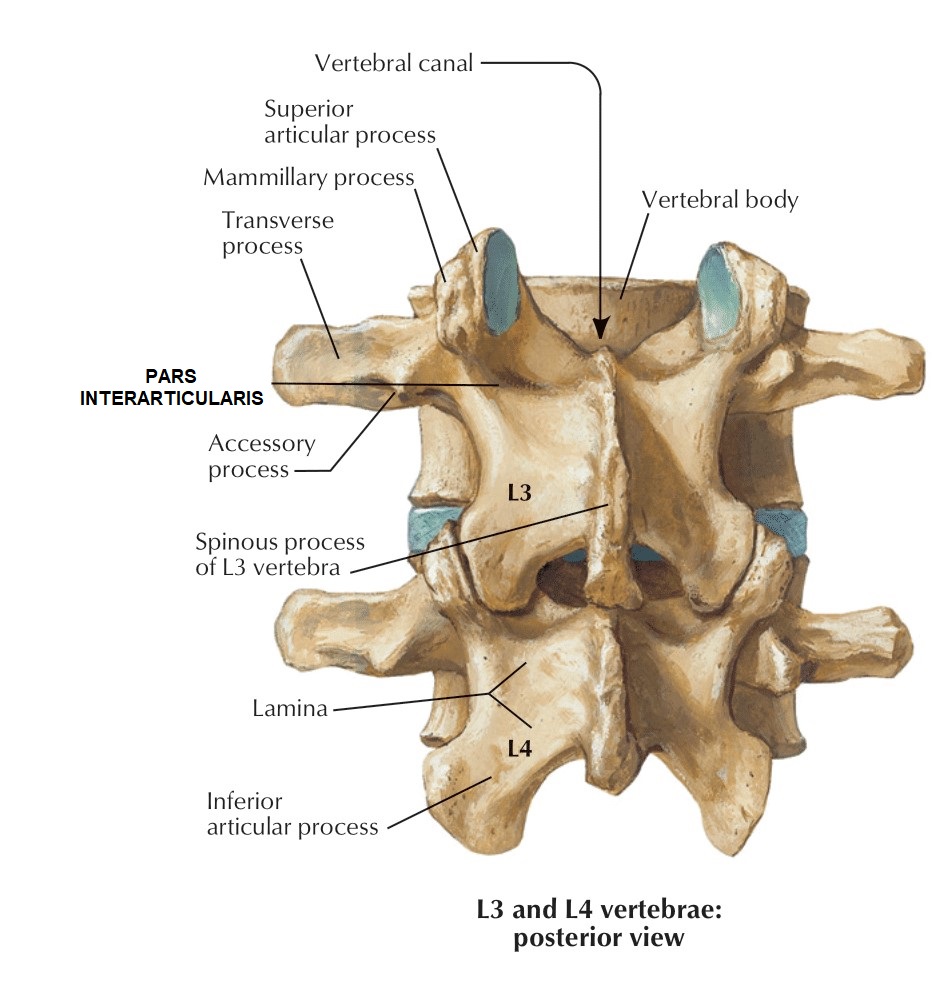
Anatomy:
Pars:
It’s a region between the superior and inferior articulating facet of the vertebra. And it is known to be the weakest area in the neural arch. That is why it is susceptible to stress fracture.
Pars defects:
Not observed in newborns or non-ambulatory patients. Lysis ( the disintegration of a cell by rupture of the cell wall or membrane) or elongation do not occur in primates that do not have an upright bipedal gait. Presence of lumbar lordosis (unique in humans) is necessary for spondylolisthesis to occur.
Classification:
· Type I: Dysplastic (child)
· Type II: Isthmic (5-50 yrs)
· Type III: Degenerative (older)
· Type IV: Traumatic
· Type V: Pathologic
Dysplastic spondylolisthesis:
dysplasia/aplasia of posterior facet joints of the L5/S1 levels. Constant spina bifida occulta at the L5 level – congenital nature. Concomitant elongation of the pars interarticularis --- frank lysis. Condition is strongly familial, with as many as a third of first-degree relatives affected with the dysplastic form.
AP view:
 |
| ‘napoleon's hat’ appearance of L5 superimposed through the sacrum. |
Isthmic spondylolisthesis
repetitive cyclical extension/torsion of the spine. Repetitive infraction fatigue failure of the pars leads to high prevalence rate. Highest biomechanical forces is applied on the pars at L5/S1 level making it the commonest site of a lytic spondylolysis.
 |
| lateral radiograph of a lytic spondylolisthesis |
 |
| Oblique radiograph of a lytic spondylolisthesis. |
Degenerative spondylolisthesis
incompetence of the posterior facet joints. 10x more common at the L4/5 than the L5/S1. It is not encountered in the under 50-year-oldindividuals. The degree of slippage in the sagittal plane is no good guide to the amount of neural compression. Also fourth dimension & time, is important
Degeneration process going on for years and years. Patients are much more readily able to adapt to neural compression than for example with a rapidly growing tumor.
ct scan:
- level of degenerative spondylolisthesis
- facet have come forward to contact the back of the vertebral body and compleely close off epidural space.
Traumatic spondylolisthesis:
Acute vertebral fractures do not occur through the pars, but through pedicles, bodies, discs. That is how so-called 'traumatic spondylolistheses' are not discrete entities. Should not be part of the generic spondylolisthesis classification according to many experts.
Pathological spondylolisthesis
metastasis and rheumatoid disease are the more common causes for this kind of spondylolisthesis. Disease of the whole motion segment rather than the pars in particular.
Low grade spondylolisthesis
low grade variety present in young adults. Frequently associated with spina bifida. Slip is characterized by translation without any angulatory or kyphotic component.
- Phalen - Dixon Sign:
Sciatic crisis typically seen in high grade adolescent spondylolisthesis. sign includes:
•
Sciatic
pain
•
Vertical
sacrum and pelvis
•
Lumbosacral
kyphosis
•
Tight
hamstrings
•
Hyperlordotic
lumbar spine
•
Waddling
gait
Back pain and spondylolisthesis
The cause of back pain is unclear and is multi-factorial.
The pain may be:
• Disc degeneration
• Facet degeneration
• Chronic nerve root irritation from compression or traction
• Patient may have accompanying spinal stenosis
Radiography:
The bending films:
demonstrate persistent motion and instability. Especially in the presence of degenerated disc disease at the level of spondylisthesis. Disc degeneration and collapse of the disc space is an attempt to stabilize the motion segment.
The bending films:
demonstrate persistent motion and instability. Especially in the presence of degenerated disc disease at the level of spondylisthesis. Disc degeneration and collapse of the disc space is an attempt to stabilize the motion segment
Radiological examination: large number of suggested and preferred radiological parameters to assess spondylolisthesis. Only 2 are of any great importance (Wiltse LL et al)
1. The amount of displacement
2. The slip angle (the angular relationship between L5 and S1 in the dysplastic form of spondylolisthesis)
Radio graphic index:
Radiological examination
Ct scan: helpful in preoperative planning especially in cases with severe dysplasia
MRI:
• assess neural foramen on the sagittal views
• determine extent of associated disc disease
• disc herniation is common(25% cases occur at the level above the slip & 15% occur at the level of the slip itself)
• Rule out tumor or infectio
Physical examination
Step off Sign-A noticable Step off sign is palpated at the Lumbo sacral area due to slippage of the vertebrae.Straight leg raise test: Straight raising of the leg with patient lying on the back causes pain and triggers the entire trunk.
Clinical presentations:
Patients typically have intermittent and localized low back pain for lumbar spondylolisthesis and localized neck pain for cervical spondylolisthesis, in increases in flexing and extending at the affected segment, as this can cause mechanic pain from motion, leading to diminished ROM (spine)
Pain may be exacerbated by direct palpation of the affected segment. And can also be radicular in nature as the exiting nerve roots become compressed due to the narrowing of nerve foramina as one vertebra slips on the adjacent vertebrae, the traversing nerve root (root to the level below) can also be impinged through associated lateral recess narrowing, disc protrusion, or central canal stenosis.
Sometimes pain and/or discomfort improve in certain positions such as lying supine. This improvement is due to the instability of the spondylolisthesis that reduces with supine posture, thus relieving the pressure on the bony elements as well as opening the spinal canal or neural foramen.
There are many other clinical features apart for these;
· Low back pain
· Atrophy of the muscles, muscle weakness
· Tense hamstrings, hamstring spasm
· Disturbances in coordination and balance difficulty in walking
· Rarely loss of bowel or bladder control
Spondylolisthesis can occur with other disorders like, spina bifida occulta, cerebral palsy, scoliosis and spinal stenosis and often seems to have a link with some of them.
Predictors of slip progression
· female gender
· prepubescence
· trapezoidal L5
· domed and vertical sacrum and sagital rotation
· slip angle > -10o
· high grade slip (>50% slip progression)
· inclined sacrum (>30o beyond vertical)
















Comments
Post a Comment